You can learn big things from something small — even something as tiny as a shrew.
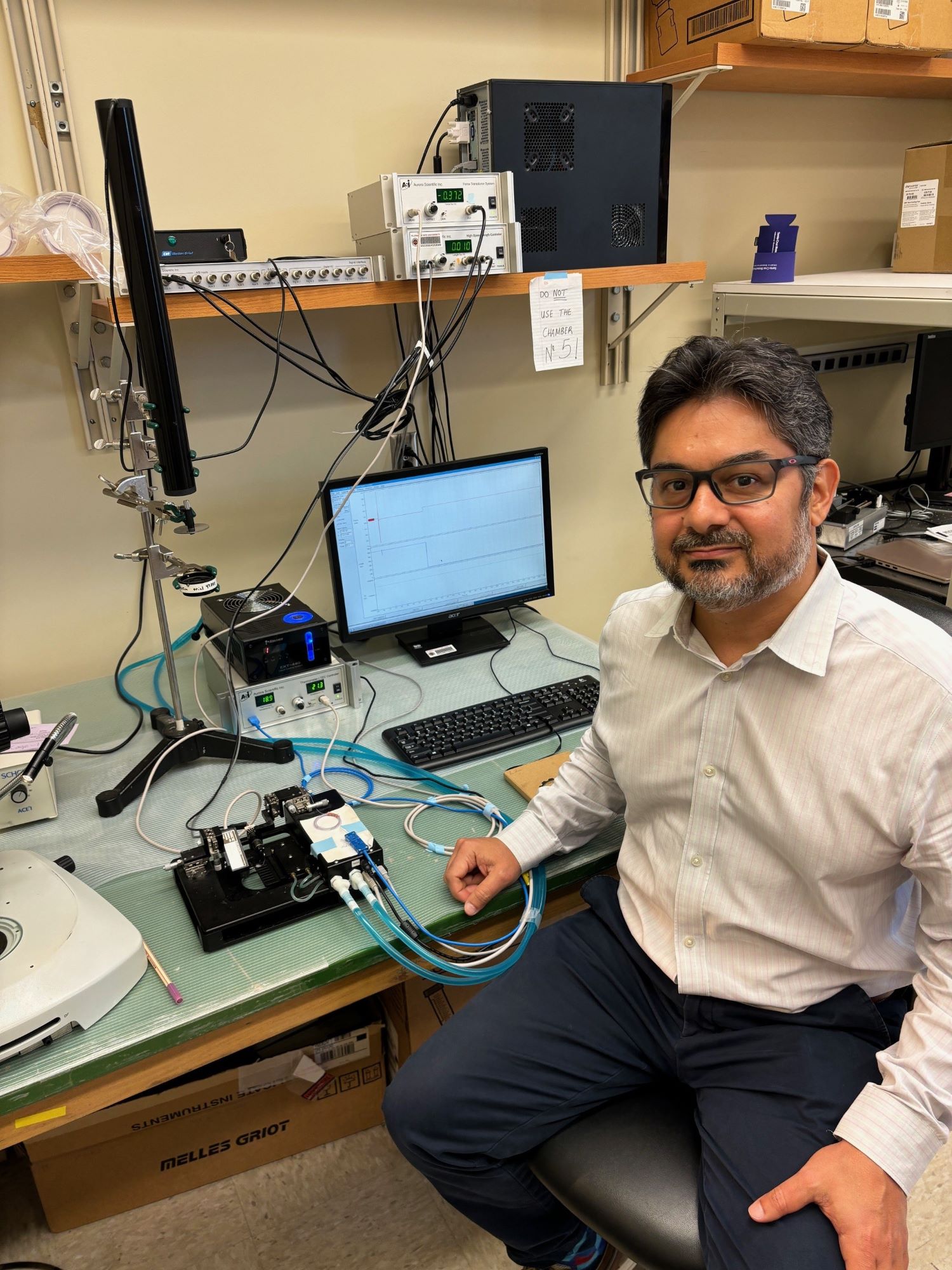
In the Sept. 27 issue of the journal Science, José Renato Pinto, Ph.D., a researcher in the FSU College of Medicine’s Department of Biomedical Sciences, provides insight into research published by a multi-national team led by William Joyce from Aarhus University, Denmark, and the University of Manchester, United Kingdom.
Pinto wrote a “Perspective” article on Joyce’s work, which focuses on a specific protein and the gene that produces it, which enable the heart to contract and relax. This research can lead to eventual treatments for people with heart disease.
To study the role specific proteins play in heart contraction and relaxation, Joyce’s team turned to shrews and moles. These small mammals, along with others such as bats, have notoriously high resting heart rates — a shrew’s heart can beat up to 1,500 times per minute. This begs the question: How can this animal’s heart beat so quickly to give the heart enough time to refill with blood for the next contraction cycle.
The answer: the TNNI3 gene and the shrew’s ability to produce a shorter form of a protein that enables the heart to relax quickly.
As an evolutionary adaptation, a small portion of the TNNI3 gene is inactivated in shrews, but not in humans. In people, the TNNI3 gene produces the full-length protein, unedited, and it possesses a different mechanism for the heart to cope with fast beats. Uniquely, bats can produce both the long and short version of the protein, as needed.
“Diastolic heart failure is common in older adults, yet, at present, there are no treatments that specifically target the root cause of impaired diastolic function,” Pinto said. “They (Joyce and team) are showing a possible solution to the problem — you could accelerate the relaxation by possibly editing the TNNI3 gene. It might be a more straight-forward, direct therapy to the root cause of the problem.”
In his article, Pinto points out that the editing and splicing of genes is already showing promise in the treatment of some types of Duchenne muscular dystrophy, but more research needs to be done.
“Basic science, including evolution-based studies, is crucial for us to understand the fundamental basis of the cells — the biological processes,” Pinto said. “If you don’t know how the proteins work inside the cell, how could you propose a new treatment for human diseases? That’s what we do here in my lab. Once we have this basic knowledge, then we can try to understand how the system is altered during diseases. And then we can propose a new therapeutic strategy. But until we understand how things work, we really can’t do anything to treat these patients or treat the root causes. We need to know how the system works.”
What makes Joyce’s work unique is that it looks to nature for solutions.
“I applaud what Joyce and the team did,” Pinto said. “I think that going back and looking at what nature did during evolution is important — and this is how I came up with the title to my article: ‘Can evolution-based studies inform modern medicine?’”
Pinto added, the way Joyce and team ended their article sums it up best: “By studying the hearts of small mammals with exceptionally high heart rates, we show that nature realized the solution to habitually accelerate diastolic relaxation long before modern biomedicine.”
Maicon Landim-Vieira, a postdoctoral fellow in the Department of Biomedical Sciences, also contributed to the “Perspective” article.