'What if?' questions could help communities tackle cancer disparities


July 2019
Imagine that a health-conscious benefactor, alarmed because substantially more black women than white women are dying from breast cancer in your community, donated a new mammography van. Smart gift, right?
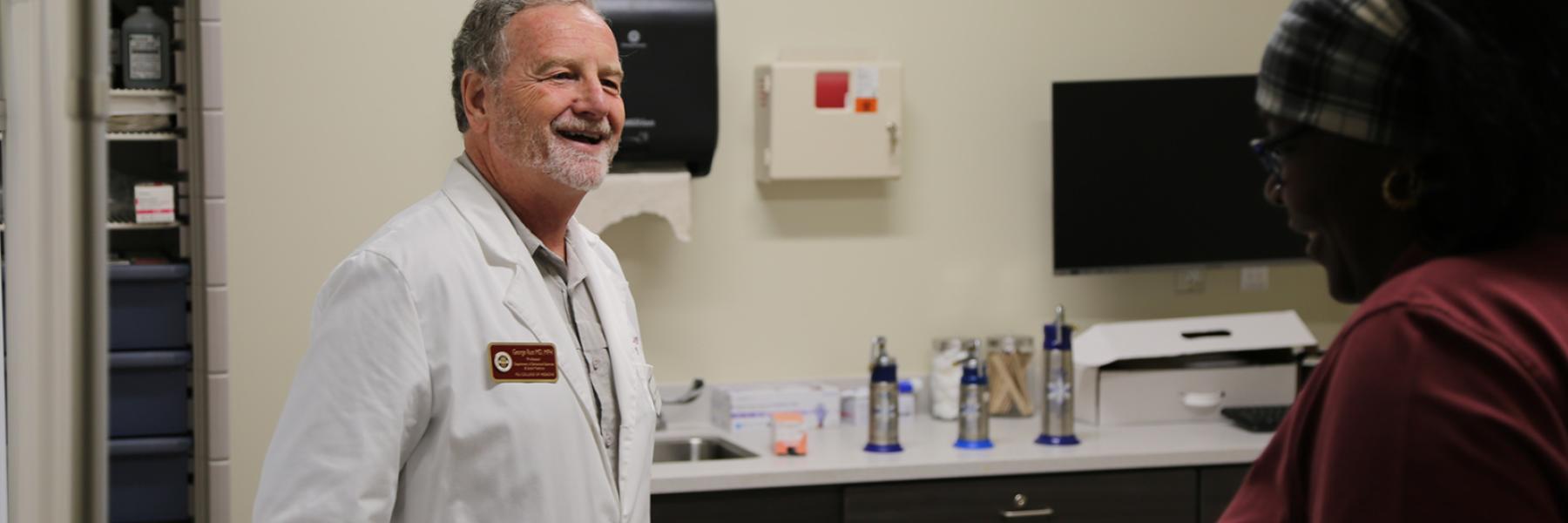
Not necessarily, says Florida State University researcher George Rust, a professor of behavioral sciences and social medicine. It’s possible that the screening rates among black and white women in that community could both be above 90 percent — so the new van would be the wrong intervention.
Finding the right intervention is what Rust’s newest project is all about. Backed by a three-year Bankhead-Coley research grant from the Florida Department of Health totaling more than $800,000, it uses big-data analytics to produce user-friendly information for any Florida community.
“While the quest continues to be to cure cancer,” Rust wrote in his project’s abstract, “the greatest opportunity for dramatically reducing cancer deaths in the next decade is more efficient use of existing innovations to achieve early diagnosis and effective treatment for all segments of the population.”
Rust is targeting what he calls two of the most screenable, treatable and curable cancers: breast and colorectal. Focusing on the gaps between whites and African Americans, he wants to provide communities with the means to find out why their specific gap exists — and then encourage them to do something about it.
“Let’s say Community A has a big screening gap — we could say, ‘Here’s your most strategic opportunity to save lives — if you could equalize those screening rates, this is how many lives you could save,’” Rust said. “In a different community, where the screening rates are equal, we might be able to say, ‘Here’s where you need to focus your efforts. Maybe it’s in partnership with hospitals and oncologists to really make sure that the new lifesaving treatments are getting equally to everyone who needs them. And that’s how many lives you could save if you did that.’”
He’s also trying to shift the national conversation by pointing out that some communities are actually eliminating some disparities. In other words, disparities are not inevitable. “We need to start holding each other accountable in getting there,” he said, “as opposed to wringing our hands and feeling powerless.”
Rust says the project, “Modeling Paths to Cancer Health Equity,” can only be done through collaboration. He is working with FSU’s statistics and geography departments, as well as health services researchers in the College of Medicine. He is also hiring a computer-simulation-modeling researcher. Penny Ralston, dean emeritus of the College of Human Sciences, will coordinate community engagement through the Health Equity Research Institute and its community partners across Florida.
“If we can develop a fairly accurate model of predicting what the death rates are for cancer — based on what the screening rate is, what the quality of treatment is, what the delays in diagnosis are — then we can play the ‘What if?’ games,” Rust said. “We can ask the computer questions such as: ‘What if we move the screening rate by this much?’ ‘What if we decrease the lag time in diagnosis by this much?’ ‘What if we increase the proportion of people who are going to a cancer center or getting the optimal cancer treatment — how much could we eliminate the gap between black and white outcomes?’”
It’s like personalized medicine, he said — except this time the community is the patient.
Using the data to build the models is crucial, of course. But for Rust, what matters most is what happens afterward.
“We envision this as a way to enhance communication and in some ways to democratize the data,” said Rust, who was founding director of the Morehouse School of Medicine National Center for Primary Care. “To have community members who are advocates and stakeholders be able to take this information and say, ‘We need to work on this part of the puzzle.’ Maybe that means rattling the cage of a hospital administrator, if people going to the same hospital are not getting the same treatment.
“Or maybe it’s that people in the community are going to this trusted hospital because it served them well over many decades but, truth be told, another hospital that maybe lost their trust has more cutting-edge cancer treatment now. Then that becomes an opportunity for community dialogue: How does the community want to handle that? Do they want to urge community members to get their care from the hospital that lost their trust? Or do they want to talk to the other hospital and say, ‘Why can’t you provide care that’s just as good as what’s being done over there?’”
The aim is to come up with an app or other tool that’s not just for academics but easily understandable in any community — one that drives action to achieve health equity.