Curriculum
Program Description:
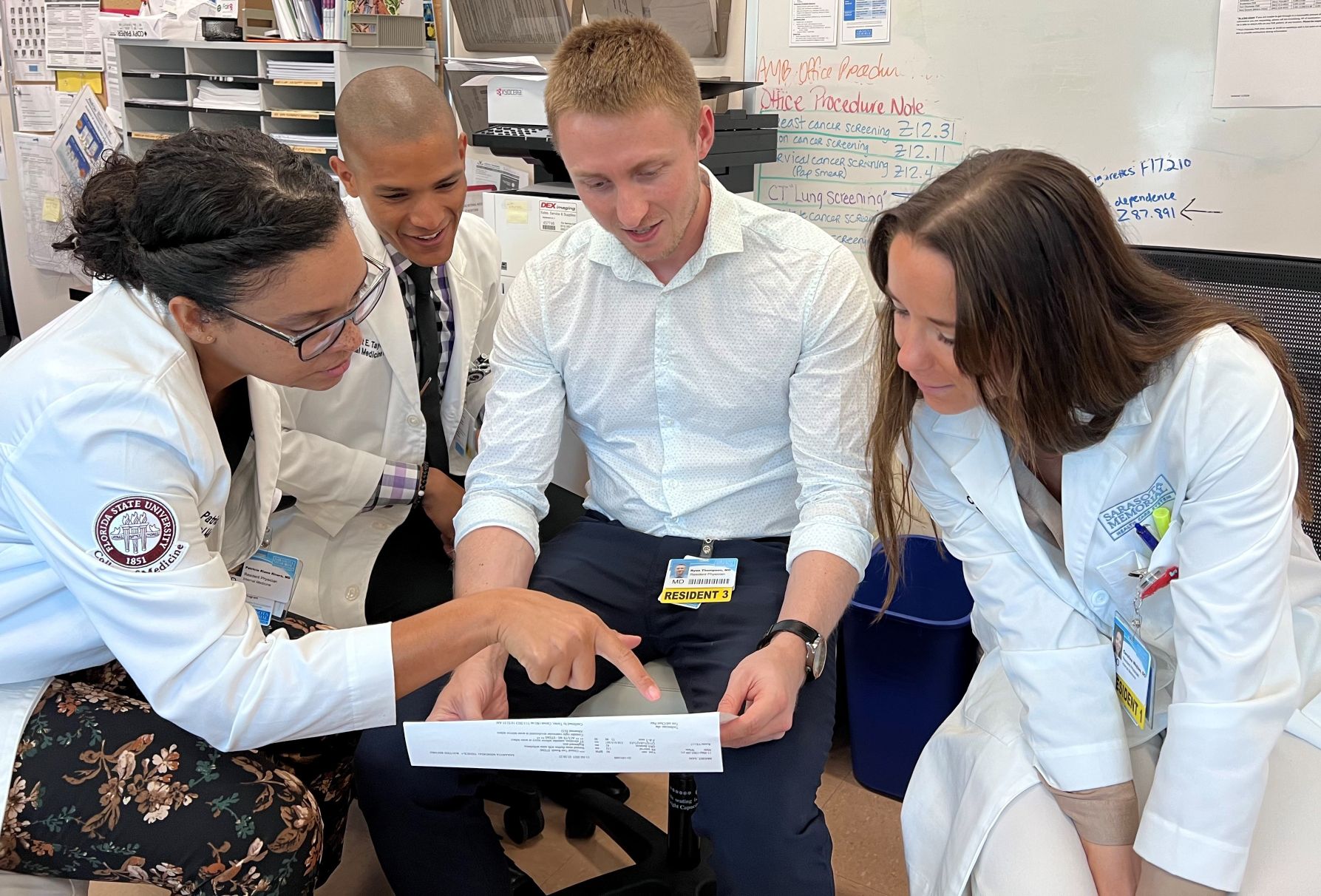
The curriculum provides a breadth and depth of clinical educational experiences in ambulatory and inpatient settings that prepare residents for careers in primary care, general internal medicine and subspecialty training.
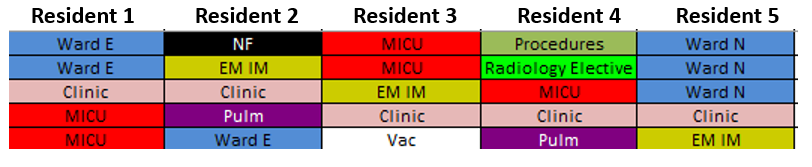
The program utilizes a “3+1” block scheduling model, whereby residents are assigned to inpatient rotations or consult services for three weeks at a time, followed by a week dedicated to ambulatory practice. This minimizes scheduling conflicts between inpatient rotations and the ambulatory experience.
All Residents have a dedicated educational session for one half-day on Wednesday afternoons (see section on Academic Half Day for more information).
| PGY1 | PGY2 | PGY3 |
|
|
|
Sample “3+1” Schedule:
Sample Continuity Week Schedule:
Clinic Week (+ 1): PGY-1 & 2
| Monday AM | Tuesday AM | Wednesday AM | Thursday AM | Friday AM |
| Clinic | Clinic | Clinic: Walk-In | Clinic | Clinic |
| Monday PM | Tuesday PM | Wednesday PM | Thursday PM | Friday PM |
| CQI/Res* | Clinic | Education Half-Day | Clinic | Admin Half-Day |
Clinic Week (+ 1): PGY-3
| Monday AM | Tuesday AM | Wednesday AM | Thursday AM | Friday AM |
| SS | Clinic | CQI | Clinic | POCUS |
| Monday PM | Tuesday PM | Wednesday PM | Thursday PM | Friday PM |
| SS | Clinic | Education Half-Day | Clinic | Admin Half-Day |
*CQI / Res: Continuous Quality Improvement Projects / Research
*SS: Subspecialty Clinic
Academic Half Day:
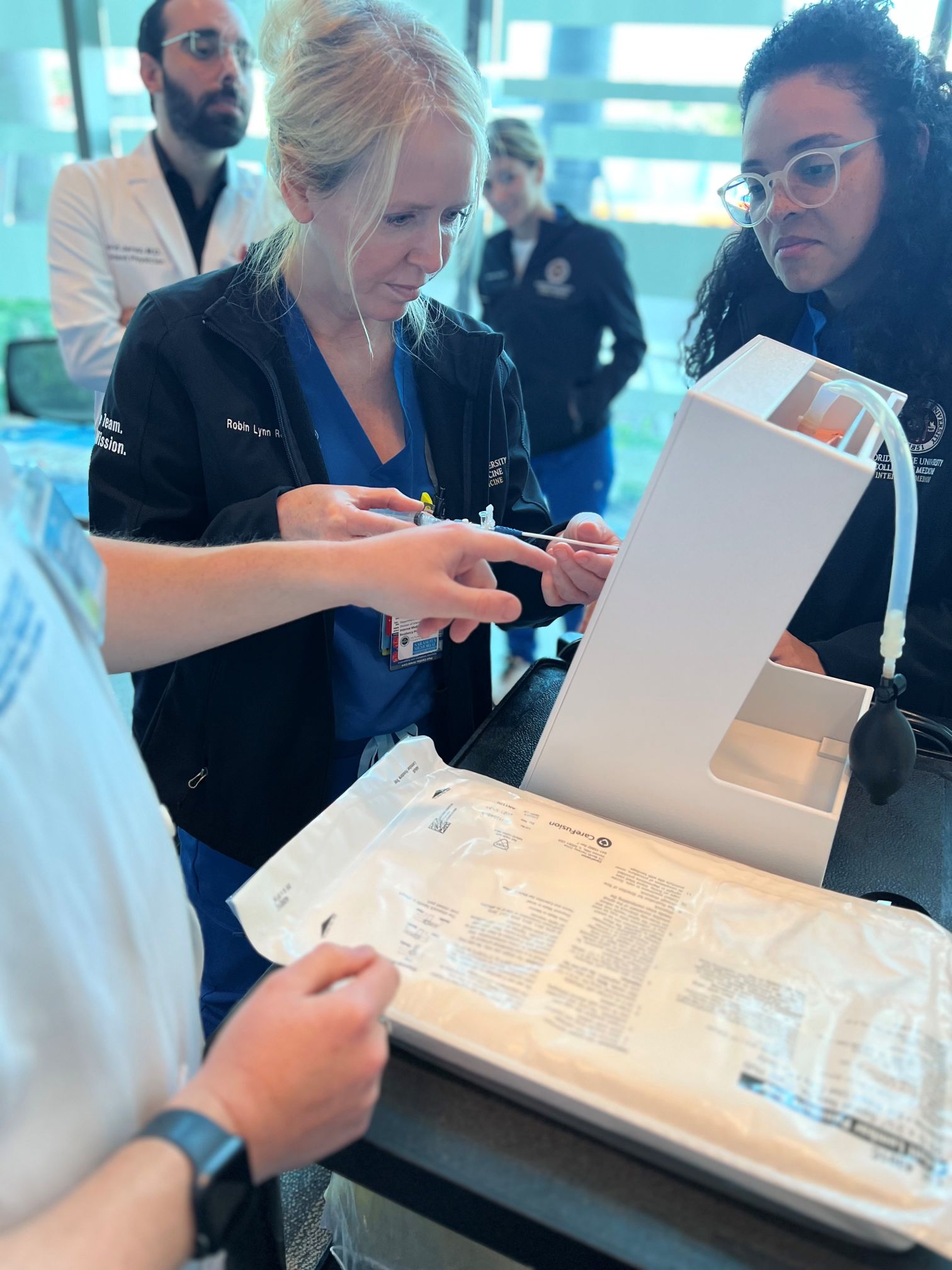
Each Wednesday afternoon contains protected time for didactics with topics that range in specialty selected based on relevance for board preparation and feedback from previous cohorts. Our faculty members participate in the delivery of a strong, longitudinal, didactic curriculum that prepares residents well for their board certifying examination. In place of Academic Half Day during the last Wednesday of each month, residents are given simulation training time with rapid response scenarios, opportunities for hands-on procedural practice, and other structured simulated learning opportunities.
Educational Goals:
The curriculum provides a breadth and depth of clinical educational experiences in ambulatory and inpatient settings to train residents to become highly competent internal medicine physicians. Throughout their training, we also help prepare residents for careers in primary care, general internal medicine, and subspecialty training.
Resources:
Our program provides access to online resources such as UpToDate, DynaMedex, Access Medicine, Lexicomp, and many more. All interns receive electronic versions of MKSAP to supplement the didactic curriculum. We also have a wealth of resources, including medical journals and texts through our affiliation with Florida State University College of Medicine.
Simulation and Immersive Learning:
SMH has an on-site Simulation Center. Residents will participate in a series of multidisciplinary team simulation exercises (mock codes, rapid response scenarios) using high-fidelity simulation equipment, coupled with Standardized Patients. In addition, FSU College of Medicine provides on-site simulation training and assessments for residents.
 |  |

