Mission Statement:
The mission of the FSU Center for Behavioral Health Integration is to strengthen the capacity of FSU to serve as an innovation leader for the state by leading and conducting research, clinical and policy programming and education/training related to behavioral health. Center activities emphasize community and medical setting research, clinical and policy enhancements aimed to improve behavioral health outcomes. The overall goal is to significantly improve outcome associated with under-addressed behavioral health disorders (i.e. mental health and substance use) in Florida and nationally.
In order to achieve its mission, the Center enhances collaboration with other professions interested in integrated health care; identify and promote the use of best practices for integrating and improving health care services; improve clinician training; improve data integration and analytics; and provide assistance to Florida’s health care providers in best practice behavioral health care.
Vision Statement:
The Center for Behavioral Health Integration is committed to promoting innovations through research and planning, and developing Florida's future physician workforce to address mental health and substance abuse issues successfully in their practice.
The Center for Behavioral Health Integration does not provide direct services, but works to improve the integration of mental and behavioral health education, research and clinical care into primary health care from a policy and systems perspective.
Center for Behavioral Health Integration Staff
 Heather A. Flynn, Ph.D.
Heather A. Flynn, Ph.D.
Heather A. Flynn, Ph.D., is a Professor at the Florida State University (FSU), College of Medicine and Chair of the Department of Behavioral Sciences and Social Medicine. She is the Director of the FSU Center for Behavioral Health Integration. Dr. Flynn received her doctorate in clinical psychology from Florida State University and completed a mental health and substance use fellowship at the University of Michigan Medical School in 1998. She served on the faculty at the UM Department of Psychiatry from 1998-2011, where she co-founded the UM Women and Infants Mental Health Program. Dr. Flynn’s research is focused on improved identification, treatment, and outcomes for behavioral health disorders, with a particular focus on women and children. As a clinical psychologist, she has worked for over 25 years as a clinician, researcher, and trainer in the behavioral health field. Her work is specifically aimed at developing and testing for behavioral health in medical and community settings. Dr. Flynn is also involved in statewide, national, and international work on improving behavioral health approaches and outcomes. She is the Co-Chair of the Florida Maternal Mental Health Collaborative and the Women & Mood Disorders Task Group Chair within the National Network of Depression Centers. She has worked with teams to develop international quality standards by implementing processes for practitioner and trainer/supervisor certifications in evidence-based behavioral health treatments, including Motivational Interviewing and Interpersonal Psychotherapy. In 2018, Dr. Flynn was appointed to serve on the Florida Governors Mental Health Task Force. She also served as a member of the Florida Statewide Suicide Prevention Task Force, and in 2020 was appointed to the Florida Governors Opioid Task Force. Dr. Flynn is passionate about community-partnered, collaborative work to improve mental health and substance use for families in the US and worldwide.
 Amandla Shabaka-Haynes, MD
Amandla Shabaka-Haynes, MD
Program Manager
Dr. Shabaka-Haynes is a Program Manager in the Department of Behavioral Science & Social Medicine Department of Florida State University’s College of Medicine. Dr. Shabaka-Haynes completed her Bachelor of Science degree at Xavier University of Louisiana and her medical training at the Latin American School of Medicine. As resource & referral specialist for the FL BH IMPACT program, Dr. Haynes’ role is to assist in evaluating the mental health, substance use, and other support service needs for providers and their patients struggling with behavioral health issues. She also serves as a liaison for providers and patients to community behavioral health resources.
 Megan Deichen Hansen, Ph.D., M.S.W.
Megan Deichen Hansen, Ph.D., M.S.W.
Assistant Professor
Dr. Megan Deichen Hansen is an Assistant Professor in the Department of Behavioral Sciences and Social Medicine at Florida State University’s College of Medicine. As a social worker and health services researcher, Dr. Deichen Hansen uses innovative methods for improving access to quality perinatal within US healthcare settings. Through this work, she aims to 1) understand mechanisms that act as barriers to care; and 2) develop and implement interventions to achieve optimal perinatal health outcomes. Her research to date has included numerous first-authored, peer-reviewed publications and presentations, including work that has contributed to ACOG (American College of Obstetricians and Gynecologists) best-practice guidance and individual practice-based training and education. In her role as a perinatal health services researcher, she has collaborated on and lead numerous community-engaged research projects, designed to advance our understanding of end users’ healthcare needs and to subsequently advance related patient outcomes.
 Monica Ragans
Monica Ragans
Program Manager
Monica is a Project Manager for the Center for Behavioral Health Integration to include Florida BH IMPACT at Florida State University College of Medicine. She is responsible for the management and implementation of projects at the Center. Monica completed her Bachelor of Science degree in Social Science at Florida State University. She has been working with the FSU College of Medicine since 2006.
 Mary Norton, MD, FAAP
Mary Norton, MD, FAAP
Pediatric Content Expert
Dr. Norton is a board certified general pediatrician with strong interests in community pediatrics, integrated behavioral health and primary care, and trauma responsive care. She completed her pediatric residency training in Greenville, South Carolina, at Greenville Children’s Hospital in 2016, then was a stay-at-home mom to her three young girls before joining the FSU College of Medicine in 2017. She has been closely involved with school based health clinics in Gadsden and Leon Counties, and was the founding pediatrician at FSU PrimaryHealth in SW Tallahassee, the medical partner of the Leon County Community Partnership School at Sabal Palm Elementary School. She currently practices general pediatrics with Tallahassee Primary Care Associates at Tallahassee Pediatrics. As pediatric content expert on the project, Dr. Norton's role is to help with engagement and retention of pediatric practices, devising processes and practices to integrate into the pediatric workflow to address behavioral health and to determine best practice pediatric behavioral health integration.
 Cori McGooden, M.S.W., L.C.S.W.,
Cori McGooden, M.S.W., L.C.S.W.,
Pediatric Program Coordinator
Cori has a bachelor’s degree in criminology and master’s degree in social work, both from Florida State University. She is a Florida licensed clinical social worker and a qualified clinical supervisor. Over the last 30 years, she has worked in the areas of youth empowerment, criminal justice, child welfare, adoptions as well as substance abuse and mental health. In 2019, Cori joined FSU’s College of Medicine. In April of that year, she became the inaugural behavioral health provider integrated into FSU Primary Health’s practice, where she focused on behavioral health integration and pediatrics. She now serves as the Project Coordinator for the Center for Behavioral Health Integration’s Hub at Whole Child Leon. Cori’s professional focus is facilitating collaboration to improve access and outcomes.
 Jasmine Max
Jasmine Max
Researcher | Flynn Lab Manager
Jasmine is the Flynn Lab Manager and Researcher for the Center for Behavioral Health Integration.
Additional Contributing Faculty and Staff

Leslie M. Beitsch, M.D., J.D.,
Courtesy Faculty, Florida State University, College of Medicine
Prior to joining the College of Medicine, Dr. Beitsch was Commissioner of Health for the State of Oklahoma, serving in that capacity from June 2001 until November 2003. Before that time, he held several positions within the Florida Department of Health for 12 years, most recently Deputy Secretary. Dr. Beitsch's focus is on Health Policy and Public Health. He previously served as Chair of the Department of Behavioral Sciences and Social Medicine and retired as Professor in August 2021. He is also affiliated with the Center for Medicine and Public Health.

George Rust, M.D., M.P.H.
Professor, Florida State University, College of Medicine
Dr. Rust joined the faculty FSU’s College of Medicine in 2016, after serving as the founding director of the Morehouse School of Medicine (MSM) Faculty Development Program and the MSM National Center for Primary Care. Previously, Dr. Rust served as the board chair of the Atlanta Community Access Coalition, co-chair of Georgia’s Minority Health Advisory Council, senior scientific advisor to the HHS Agency for Healthcare Research and Quality (AHRQ), and Medical Director for the West Orange Farmworkers Health Association. Dr. Rust received his medical degree from Loyola University Stritch School of Medicine, and completed residency training in Family Medicine at Cook County Hospital in Chicago. He is board-certified in both Family Practice and in Preventive Medicine. Dr. Rust is the author of over 100 peer-reviewed publications, book chapters and monographs, and is the recipient of numerous local, state, and national awards for teaching and service. His career as a family physician and scholar has consistently focused on primary health care and community health for those in greatest need, and on the elimination of health disparities and on charting a path to health equity.

Jeffrey Harman, Ph.D.
Professor, Florida State University, College of Medicine
Dr. Harman, a health economist, is a Professor in the Department of Behavioral Sciences and Social Medicine at the Florida State University College of Medicine in Tallahassee, Florida. After working for several years as a mental health counselor, he received his Ph.D. in Health Services Research, Policy and Administration from the University of Minnesota. His research explores utilization and expenditures of health services, with an emphasis on the impact of health policies on services for vulnerable populations, such as Medicaid beneficiaries and individuals suffering from mental illness. In the past five years, Harman’s research examining these issues have been funded by such agencies as the National Institute of Mental Health, National Institute on Alcohol Abuse and Alcoholism, the Robert Wood Johnson Foundation, Florida’s Agency for Health Care Administration, and private industry. Dr. Harman’s research has resulted in over 85 peer-reviewed scientific articles. He has been a grant reviewer for such organizations as the National Institutes for Health and the Agency for Healthcare Research and Quality, and serves as a reviewer for over 20 journals, having been designated an Exceptional Reviewer on multiple occasions.

Samantha Goldfarb, Dr.P.H.
Assistant Professor, Florida State University, College of Medicine
Dr. Goldfarb joined the FSU College of Medicine in 2015 as Research Faculty in the Department after graduating from University of Alabama at Birmingham School of Public Health with a Doctorate of Public Health (DrPH) in the Department of Health Care Organization and Policy. Dr. Goldfarb’s degree holds a concentration in Maternal and Child Health Policy, and her research is focused on these issues, particularly as they relate to the life course perspective which holds that there are a complex set of risk (e.g., stress, perceived discrimination) and protective (e.g., education, mental health counseling) factors that impact individuals’ health throughout their life span which must be addressed for optimal prevention of poor health outcomes. She is particularly interested in understanding the impact of state health and drug policies on maternal and perinatal populations. She has assisted in teaching master’s level public health courses related to conducting research, community-based needs assessments, and program evaluations. She has also been involved in several state and federal contracts in both Florida and Alabama aimed at improving population health through surveillance and assessment.

Heidi Kinsell, Ph.D.
Assistant Professor, Florida State University, College of Medicine
Dr. Kinsell is an Assistant Professor in the Department of Geriatrics in the College of Medicine at Florida State University. Dr. Kinsell is a health services researcher who examines access, utilization, and quality of care for vulnerable and aging populations with an emphasis on improving behavioral health treatment. Additional research interests include exploring the relationships between quality of care and provider staffing in post-acute and long-term care settings and the effects of health policies on population outcomes using various economic frameworks.
.jpg)
Tyra Dark, PhD
Assistant Professor, Florida State University, College of Medicine
Dr. Dark, a chronic disease epidemiologist, is an Assistant Professor in the Department of Behavioral Sciences and Social Medicine at the Florida State University College of Medicine in Tallahassee, Florida. Dr. Dark is specifically interested in the comorbidity of mental illness and cardiometabolic syndrome, identifying the unique health care needs of this population, and the role of race/ethnicity on delivery of care. Her current research focuses on identifying how care is delivered to this population to uncover potential contributors of racial/ethnic disparities that can inform future policy or other health care delivery interventions to improve outcomes and reduce observed disparities. She has conducted several studies focused on examining emergency department visits for anxiety disorders, including an epidemiologic assessment of the content of care during those visits. This research has resulted in the submission and publication of scientific articles highlighting these study findings. Additionally, she received the Robert Wood Johnson Foundation New Connections award allowing her to continue research in the area of cardiometabolic syndrome and comorbid anxiety disorder. Dr. Dark will apply this knowledge and insight to health services research to examine influences on the delivery of health care.
In Memoriam, Harold Robert (Bob) Sharpe, MSW
 Harold Robert (Bob) Sharpe, MSW, who created the initial vision for the FSU Center for Behavioral Health Integration, died on December 23, 2015. Bob devoted his career and retirement to health care work for the underserved. He founded the FSU Center for Behavioral Health Integration by establishing a partnership between the FSU College of Medicine Behavioral Sciences and Social Medicine Department and the Florida Council for Community Mental Health. Bob created a vision and strategic plan for the Center for Behavioral Health Integration that aimed to improve the integration of mental and behavioral health education, training, research and clinical care into primary health care. Bob’s work and ideas were vital to the creation of the Center.
Harold Robert (Bob) Sharpe, MSW, who created the initial vision for the FSU Center for Behavioral Health Integration, died on December 23, 2015. Bob devoted his career and retirement to health care work for the underserved. He founded the FSU Center for Behavioral Health Integration by establishing a partnership between the FSU College of Medicine Behavioral Sciences and Social Medicine Department and the Florida Council for Community Mental Health. Bob created a vision and strategic plan for the Center for Behavioral Health Integration that aimed to improve the integration of mental and behavioral health education, training, research and clinical care into primary health care. Bob’s work and ideas were vital to the creation of the Center.
Bob also served on the Maternal Mental Health Community Advisory Board, working closely with the FSU Department of Behavioral Sciences and Social Medicine and several leaders and stakeholders in the community. Bob’s wealth of experience in health care provided immeasurable and valuable guidance for the work of the FSU Center and for our Mental Health initiatives and programs.
Bob served as president and chief executive officer of the Florida Council for Community Mental Health and its advocacy organization, the Florida Council for Behavioral Health Care. The Councils represent nearly 60 community-based behavioral health treatment organizations throughout Florida. He joined the Council in 2004, following a distinguished career in Florida government. He obtained his master’s degree in social work from Florida State University and a bachelor’s degree in criminology from Florida State University. He began his career as a social worker in Washington, D.C. in 1970, and soon moved to Florida, where his career in health and human services has encompassed a number of positions in the field of health and human services.
Immediately prior to taking the helm of the two behavioral health associations, Bob served as Deputy Secretary for Medicaid at the Florida Agency for Health Care Administration. Prior to heading up Florida’s Medicaid Program, he served as the Assistant Deputy Secretary for Medicaid and Director of Health Policy at the Agency. Earlier in his career, Bob served in a number of key positions at the former Florida Department of Health and Rehabilitative Services. These include director of the Office of Health Planning and Chief of the Medicaid Program Analysis Bureau.
Bob had an incredible passion for creating programs and policies to improve quality care for individuals living with mental illness in Florida. He worked tirelessly into his retirement. Bob’s vision and passion will continue to guide the work of the FSU Center for Behavioral Health Integration, and will carry us forward in our efforts to improve suffering among the underserved for years to come. He will be greatly missed.

The FL BH IMPACT (Improving Maternal and Pediatric Access Care and Treatment) program is aimed to enhance the capacity of perinatal and pediatric clinicians to improve behavioral health outcomes in Florida and beyond. The program partners with clinicians and clinical care sites to integrate screening, training and technical assistance, as well as access to behavioral health specialists including psychiatric access.
Our program has two active programs that seeks to enhance accessibility of resources for patients and families in need of mental health and substance use supports: Maternal & Perinatal Mental Health Program and Pediatric Behavioral Health Program. These program also provide a statewide directory of active and qualified maternal and pediatric behavioral health providers. BH Impact operates under the Florida State University Center for Behavioral Health Integration.

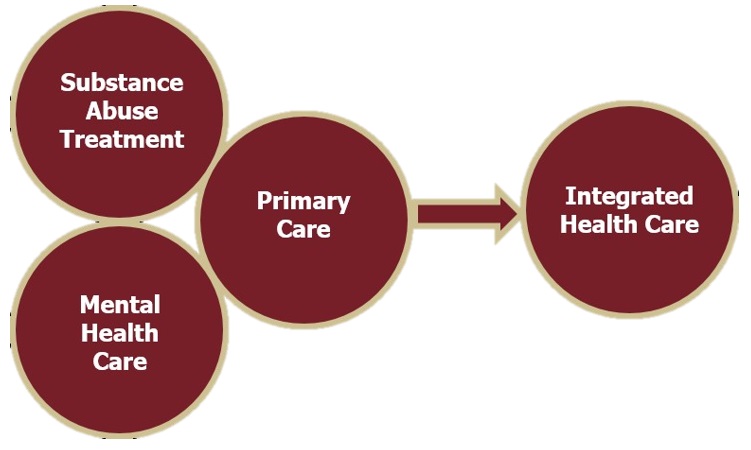
What is Integrated Care?
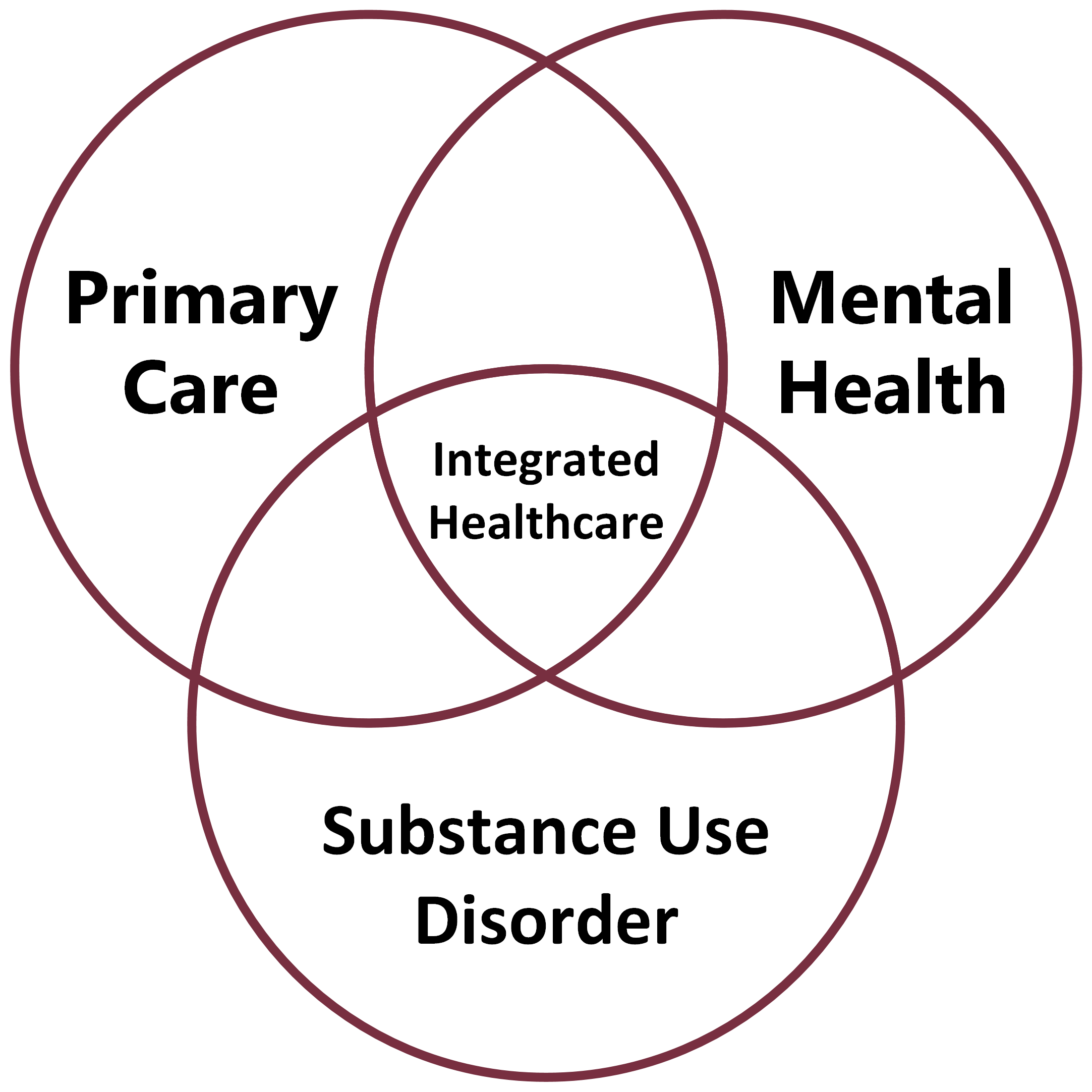
People with mental and substance use disorders may die decades earlier than the average person — mostly from untreated and preventable chronic illnesses like hypertension, diabetes, obesity, and cardiovascular disease that are aggravated by poor health habits such as inadequate physical activity, poor nutrition, smoking, and substance abuse. Barriers to primary care — coupled with challenges in navigating complex health care systems — have been a major obstacle to care.
At the same time, primary care settings have become the gateway to the behavioral health system, and primary care providers need support and resources to screen and treat individuals with behavioral and general health care needs.
The solution lies in integrated care—the systematic coordination of general and behavioral health care. Integrating mental health, substance abuse, and primary care services produces the best outcomes and have been proven to be the most effective approach to caring for people with multiple health care needs.
By providing medical and mental/behavioral health services, integrated health care aimes to address the whole person, not just one aspect of the consumer’s health care needs. In this model of care, medical and behavioral providers collaborate to coordinate the assessment, treatment, and follow-up of both mental and physical health conditions. Integrated health care reflects a holistic approach to health care that is strengths-based and person-centered and represents an opportunity to improve care and reduce costs.
Key Elements of Integrated Health Care
- A comprehensive screening and assessment.
- Identification of a patient-centered physical and behavioral health “home” that provides opportunities for collaboration and co-location of services.
- The shared development and communication of care plans.
- Care coordination and management to ensure quality care and provide support for consumers and providers.
- Engagement of consumers in self-management and care planning.
Source: SAMHSA-HRSA Center for Integrated Health Solutions, accessed 2015
Why is Integrated Health Care important?
Co-occurrence of chronic medical disorders and complex health needs are an expectation, not an exception for the severe and persistent mental illness (SPMI) population (NASMHPD, 2008).
Mental illnesses are among the world’s most costly and burdensome conditions. Florida lags behind the nation in services, training and research funding in mental health.
- Florida is the 3rd largest state, but it ranks 50th in the nation in per capita mental health spending.
- Mental illness is a leading cause of disability in the U.S. for ages 15-44. By 2020, major depressive illness is expected to be the leading cause of disability in the world for women and children.
- Behavioral health conditions commonly co-occur with other chronic health conditions in adults but services are rarely coordinated. The shortage of both behavioral health and primary care providers in many areas makes the provision of care, particularly integrated services, difficult.
- Behavioral health conditions commonly co-occur with other chronic health conditions in adults and yet services are rarely delivered in coordination.
- People with serious mental illness die 25 years earlier from common medical conditions such as cancer and heart disease, making this among the most glaring health disparities in our nation.
- Americans with severe mental illness spend 2 to 3 times more on health care than other patients, often due to late diagnosis and delayed treatment.
- In spite of effective prevention, treatment and recovery, behavioral health conditions are under-diagnosed and under-treated in the U.S.
- On average, 45% of suicide victims had contact with primary care providers within one month of suicide, and 75% of suicide victims had contact with primary care providers within the preceding year.
Mortality Crisis
- U.S. Life Expectancy 2008 = 78 Years
- Seriously Mentally Ill = 53 – 57 Years
- Comparable to Cameroon, Gabon, Democratic Republic of Congo
- Biggest Lifespan Disparity in U.S.: 21-25 Years
Source: Massachusetts Department of Mental Health, 6/09
High Rates of Chronic Illness
• 70% of SPMI Population Have a Chronic Health Condition
• Mostly Pulmonary Disease/Lung Cancer/Diabetes
• 50% Have Two or More Chronic Conditions
• 42% Have Conditions Severe Enough to Limit Function
• Hepititis B Rates 5 times higher; Hepititis C Rates 11 times higher
Source: National Association of State Mental Health Program Directors, 10/06
U.S. Health Delivery System
- The dominant models of providing health care in the United States separate the mind and body
- Separation has a negative impact on health care access, health care costs, and quality of care with a disproportionate share of the burden falling on women, the elderly, racial and ethnic minorities, and rural and immigrant populations
Source: Health Care for the Whole Person Statement of Vision and Principles, American Psychological Association
What are the Problems with the Traditional System
There are barriers to integrated care on multiple levels including clinical, financial, policy and organizational. These include:
- Fragmentation of care due to the physical separation of providers
- Separation of medical records, i.e., “the left hand doesn’t know what the right hand is doing”
- Limited communication between medical and mental health providers
- Primary care is often responding to multiple presenting problems creating time management issues
- Primary care providers often have limited training in psychiatric disorders and their treatment; half of those with mental disorders go undiagnosed in primary care
- Primary care patients often have limited access to specialty mental health providers
Source: Meland, Prime West Health System
Behavioral Health Integration Resources
Online Mental Health Resource Guide
Through a collaboration with the United Way Big Bend and 2-1-1 Big Bend, the College of Medicine developed and maintains an online directory of mental health and social service providers in Tallahassee and the surrounding regions. To assist local clinicians with making appropriate referrals for their patients, this free and public database is searchable by the providers' specialties as well as the insurance that they accept in order to ensure that patients' complex health care needs are met in a personalized manner that best fits their situation. Mental health and social service providers are also able to request an update of their information or to be added to the list if they are not already included.
You can visit the site here: 211 Big Bend Mental Health Directory Search
Florida Maternal Mental Health Resource Directory
If you or someone you know is looking for support for your mental and behavioral health, please visit our Florida Maternal Mental Health Resource Directory to search for active and qualified maternal mental and pediatric health providers. That includes help with post-partum depression, anxiety, substance use disorder, and other conditions. You will be able to search and connect with services that fit your personal healthcare desires, preferred payment type, insurance status, and location.
We also welcome clinicians and other providers seeking resources for their patients.